Vein Clinic:
‑ Ultrasound Evaluation‑ Sclerotherapy
‑ Mini‑Phlebectomy
‑ Endovenous Laser Therapy

Our Vein Clinic is a state-of-the-art facility providing the latest technological advances in vein treatment, specializing in Endovenous Laser Therapy.
More info...
Hernias
Certain areas of the abdomen wall may be naturally weaker leading to the development of hernias. Hernias can develop at these or other areas due to heavy strain on the abdominal wall, aging, injury, an old incision, or a weakness present from birth. People of both sexes and all ages are at risk of hernias. Whereas the majority of hernias in children are congenital, hernias in adults result from a natural weakness or strain from heavy lifting, persistent coughing, difficulty with bowel movements or urination can cause the abdominal wall to weaken or separate. Unfortunately, a hernia does not get better over time, nor will it go away by itself. A hernia occurs when the inside layers of the abdominal muscles have weakened, resulting in a bulge or tear. In the same way that an inner tube pushes through a damaged tire, the inner lining of the abdomen pushes through the weakened area of the abdominal wall to form a small balloon-like sac. This can allow a loop of intestine or abdominal tissue to push into the sac. The hernia can cause severe pain and other potentially serious problems that could require emergency surgery.
A hernia occurs when the inside layers of the abdominal muscles have weakened, resulting in a bulge or tear. In the same way that an inner tube pushes through a damaged tire, the inner lining of the abdomen pushes through the weakened area of the abdominal wall to form a small balloon-like sac. This can allow a loop of intestine or abdominal tissue to push into the sac. The hernia can cause severe pain and other potentially serious problems that could require emergency surgery.Hernias occur most commonly in the groin (inguinal), belly button (umbilical), and the site of a previous operation (incisional). You may feel pain when you lift heavy objects, cough, strain during urination or bowel movements, or during prolonged standing or sitting. In addition, a bulge under the skin may be noticed. The pain experienced may be sharp and immediate or a dull ache that gets worse toward the end of the day. Severe, continuous pain, redness, and tenderness are signs that the hernia may be entrapped or strangulated. In the case of such symptoms, immediately contact your physician or surgeon.
Recommended Treatment
We recommend Laparoscopic repair for the all types of hernias. Laparoscopic hernia repair is similar to other laparoscopic procedures. A person undergoing a laparoscopic hernia repair is given general anesthesia, followed by an incision usually in or just below the belly button. Carbon dioxide is used to inflate the abdomen in order to separate the abdominal organs and provide the surgeon a clearer view of the abdominal organs and prevent them from injury. The surgeon then inserts a laparoscope and another instrument through the small incision. A laparoscope is a long, thin, metal device with a light and magnifying lens. The laparoscope allows the surgeon to see the hernia and affix a mesh patch behind the abdominal muscle wall with titanium staples. The patch rests against the thin inner lining of the abdomen.
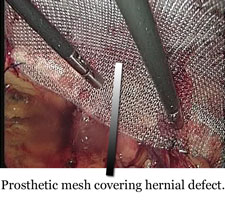 For the Inguinal hernias we prefer a Totally Extraperitoneal (TEP) approach – only the preperitoneal space is entered during the operation, without entering the abdominal cavity. As a result, the possibility for injury of the inner abdominal organs is very low. A special mesh patch is usually placed in the preperitoneal space and titanium staples are not required for the mesh fixation. This is probably the most physiological repair although technically more demanding. A fast recovery with minimal pain is anticipated, allowing a quick return to normal daily activities. Using this method, we can perform bilateral hernias repair without the need for additional incisions.
For the Inguinal hernias we prefer a Totally Extraperitoneal (TEP) approach – only the preperitoneal space is entered during the operation, without entering the abdominal cavity. As a result, the possibility for injury of the inner abdominal organs is very low. A special mesh patch is usually placed in the preperitoneal space and titanium staples are not required for the mesh fixation. This is probably the most physiological repair although technically more demanding. A fast recovery with minimal pain is anticipated, allowing a quick return to normal daily activities. Using this method, we can perform bilateral hernias repair without the need for additional incisions.Following the operation, the patient is transferred to the recovery room for 1-2 hours of monitoring, until fully awake. Once awake and able to communicate, the patient is sent home. In the 24-48 hours following a hernia operation, some soreness may be experienced. Patients are encouraged to be up and about the next day. Patients are usually able to engage in their normal activities following a short amount of time after the operation.
You should notify your surgeon or your family doctor if the following appear:
- Lasting fever over 39°C, bleeding, increasing abdominal swelling, pain that in not relieved by the medications, persistent nausea or vomiting, inability to urinate, chills, persistent cough or shortness of breath, purulent drainage (pus) from any incision, redness surrounding any of your incisions that is worsening or getting bigger.
Back to Minimally Invasive Surgery main page.
Contact Us
Minimally Invasive Surgery:
‑ Appendix‑ Bowel
‑ Gallbladder
‑ Gastro‑esophageal Reflux
‑ Hernias
‑ Rectum & Anus
‑ Spleen
‑ Varicose Veins
Endoscopy:
‑ Gastroscopy‑ Colonoscopy
Other:
‑ Breast‑ Thyroid